FACT SHEET
FOR IMMEDIATE RELEASE
June 21, 2016
Contact: CMS Media Relations
(202) 690-6145 | CMS Media Inquiries
Strengthening the Marketplace
by Covering Young Adults
Deploying New Targeting Strategies and Partnerships to Reach
Young Adults and Others Who Are Still Uninsured
Deploying New Targeting Strategies and Partnerships to Reach
Young Adults and Others Who Are Still Uninsured
With millions of Americans
insured through the Health Insurance Marketplaces, it's clear that Marketplace
coverage is a product consumers want and need as well as an important business
for insurers – with several major issuers expanding their Marketplace presence.
At the U.S. Department of Health and Human Services (HHS), we are constantly
monitoring the health of the Marketplace and are always looking to make
improvements that benefit both consumers and issuers. Over the past several
months, HHS has taken a series of actions to
strengthen the Marketplace risk pool, and
ensure a strong Marketplace
for the long term. As part of our continued commitment to the long-term
strength of the Marketplace, earlier this month, HHS made announcements regarding
additional efforts to strengthen the Marketplace risk pool and new
work with insurers and
state Departments of
Insurance to improve coverage options.
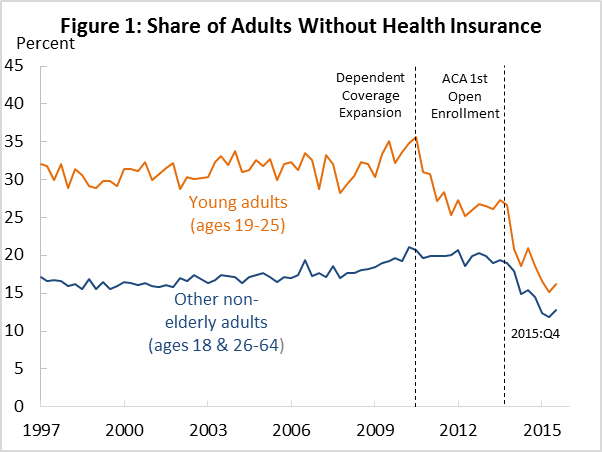
Since the ACA was enacted, the
overall uninsured rate has fallen by more than 40 percent, and the uninsured
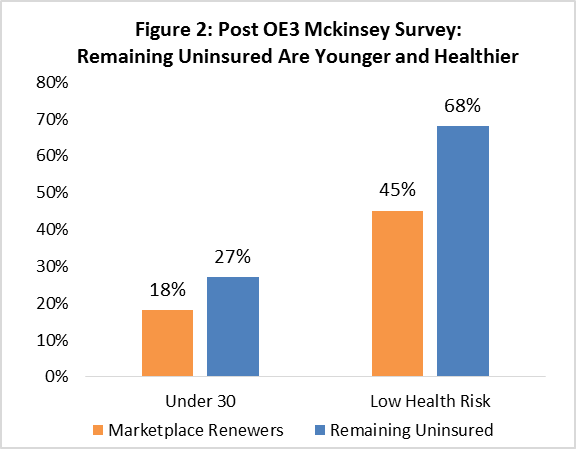
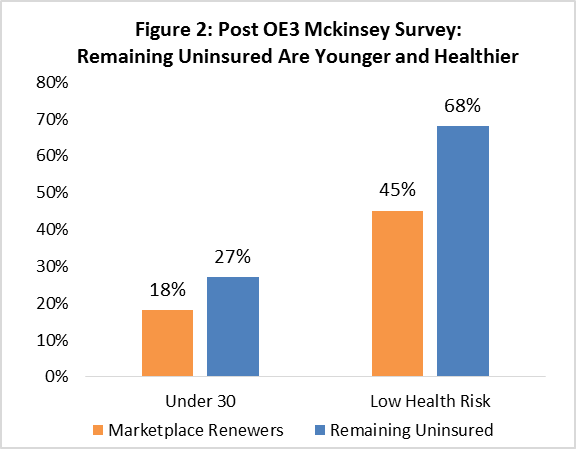
rate among young adults has fallen by more than half (see Figure 1). But
younger and healthier adults are still more likely than average to remain
uninsured (see Figure 2). Insuring these groups lets them invest in their
health, protects them against catastrophic costs from serious illness,
and helps young adults
continue their education. It also contributes to a more balanced
Marketplace risk pool and lower costs.
Today, we are announcing a series
of actions to step up Marketplace outreach, especially to young adults, for the
2017 Open Enrollment. Highlights include:
·
New outreach to uninsured people who paid the individual
responsibility penalty. For the first time this fall, we will conduct outreach to
individuals and families who paid the fee for being uninsured, or claimed an
exemption from that fee, for 2015. Young adults are overrepresented among those
who paid the fee, and healthier individuals of all ages presumably are as well.
This new outreach strategy, which has been recommended by outside experts and is already in use in Massachusetts, will let us
directly reach millions of people who were recently uninsured and may newly
appreciate the value of Marketplace coverage.
·
Smarter outreach during Open Enrollment, especially to young
adults. Research during the 2016 Open Enrollment showed that young adults
are almost twice as likely as older consumers to enroll because they receive an
email about Marketplace coverage. During the upcoming Open Enrollment, we will
draw on lessons learned this year about the messages, timing, and tactics that
make email outreach more effective. Also, new since the 2016 Open Enrollment,
this year we will be able to email consumers in near-to-real time if they open
an account but don’t start an application, start an application but don’t
finish, or select a plan but don’t pay their first premium. We’ve learned
that sending an email, with the right information, at just the right time, can
make a significant difference in whether someone gets covered, and those are
lessons we’ll act on this year.
·
Facilitating young adults’ coverage transitions. Today, we are making it easier for issuers to
conduct outreach to young adults turning age 26 and moving off their parent’s
plans. Specifically, new guidance from the Department of Labor makes clear that
the sponsors of employer plans can – and are encouraged to – provide additional
information that will help young adults understand their options and enroll in
Marketplace coverage as appropriate. Along with issuing new policy guidance, we
are strongly encouraging insurers to contact these consumers with targeted
information about Marketplace options. Additionally, on June 13, we provided states and outreach organizations
with $32 million in additional funding to help with Medicaid and Children’s
Health Insurance Program (CHIP) outreach. In conjunction with that funding
announcement, we reminded them of their obligation to help children aging out
of Medicaid and CHIP transition to Marketplace or other coverage.
·
Public-private partnerships to engage young adults. HHS has created a network of diverse outreach
partners. While we will keep building that network until the start of the 2017
Open Enrollment and beyond, we are excited to announce that this year’s
partnerships will include:
o
Lyft: New this year, Lyft will develop user discount
codes for people utilizing the ride-sharing service to attend Open Enrollment
events where they can receive assistance signing up for coverage via the ACA.
In addition, Lyft will again amplify enrollment deadlines and the importance of
getting health insurance via the ACA to their drivers in 190 cities.
o
American
Hospital Association: Along with other
actions, the American Hospital Association will develop a social media toolkit
that hospitals may use to reach young adults in their communities to educate
them about health insurance, how to enroll in the Marketplace, where to go for
enrollment assistance, and information about subsidies.
o
Coordinated
young adults campaigns.
Along with more than 75 partnering organizations, Enroll America, Young
Invincible, and Out2Enroll are announcing four targeted campaigns for the 2017
Open Enrollment. These campaigns are aimed at reaching the broad population of
young adults, community college students, young families, and LGBTQ youth. To
help focus these efforts, the White House will host a National
Millennial Health Summit on September 27, 2016.
SECTION I: NEW STRATEGIES FOR OPEN ENROLLMENT
Outreach to Penalty Payers and Others Who Were Recently Uninsured
When consumers without health insurance file their taxes, they must either pay a fee for not having health insurance, or claim an exemption from the fee. In 2014, 7.9 million filers paid the fee, and millions more claimed an exemption, including some who could be eligible for substantial financial assistance through the Marketplace. About 45 percent of taxpayers paying a penalty or claiming an exemption were under age 35, compared to about 30 percent of all taxpayers in 2014.
Outside experts have suggested reaching out to those who paid the fee or claimed an exemption to make sure they are aware of their options to enroll in coverage. In Open Enrollment 3, the Massachusetts Health Connector asked the Massachusetts Department of Revenue (DOR) to send a special mailing to Massachusetts residents that self-reported on their Massachusetts tax returns that they are without health insurance coverage. DOR sent a mailing to approximately 115,000 residents around the Commonwealth, letting them know about the affordable coverage available through the Health Connector and where to get free, in-person help to get enrolled.
For the first time this Open Enrollment, CMS will partner with IRS to conduct outreach to families that paid the fee or claimed an exemption for 2015. This will help us reach a group of individuals who were recently identified as uninsured, and who are likely to be most interested in Marketplace enrollment. We will incorporate targeted messages that reflect their recent experience with the penalty and potential eligibility for financial help.
Targeted outreach to this group is likely to be highly effective:
- In other contexts, heightening awareness of the fee for
going without health insurance increases enrollment; for example,
including information about the penalty in outreach emails increased
enrollment in response to these emails by 13 percent.
- For low- and moderate-income families who either paid
the fee or claimed exemptions last year, outreach can provide targeted
information about financial assistance. Research during the most recent
Open Enrollment showed that this is among the most effective messages in
driving enrollment for almost all groups of consumers, including young
people.
Learning from the 2016 Open Enrollment Period
During the previous Open Enrollment, we learned a number of important lessons about how to reach young adult consumers. Among them, young adults are more responsive to email than other consumers– about twice as likely to enroll in response to email outreach as older individuals.
Fortunately, we’ll be starting the 2017 Open Enrollment with the benefit of new functionalities and new data that will make our email outreach more effective. Improvements include:
- New features to
support more effective email outreach. Consumers are more
likely to respond to emails that tell them exactly what they need to do
next and reach them when they are in the process of trying to get
coverage. Since the 2016 Open Enrollment, we’ve developed new
functionalities that let us email consumers in near-to-real-time about how
to complete the next step in their enrollment process. For example, a
consumer who creates an account will receive an email about how to enroll;
a consumer who completes an application will receive an email letting her
know she needs to pick a plan; and a consumer who selects a plan will
receive an email telling her how to pay her first premium.
- A better understanding of what works to reach different
consumers. Research during
the 2016 Open Enrollment showed that providing information about financial
assistance is among the most effective messages for getting consumers to
enroll. In addition, emails informing consumers about premium increases in
their current plan and the potential benefits of shopping for a new plan more
than tripled the share of consumers coming back to the Marketplace to
actively renew their coverage.
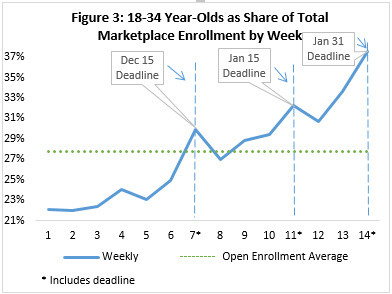
We’ve also learned that young
adults are far more deadline sensitive than other consumers (see Figure 3).
That information will influence how we time our email, television, and other
forms of outreach to young adults for the upcoming 2017 Open Enrollment. Next
year, we’ll structure our outreach to people when we know they’re paying
attention and are most likely to enroll.
SECTION II: PREVENTING THE LOSS OF HEALTH COVERAGE FOR YOUNG ADULTS AS THEY AGE
The Affordable Care Act has contributed to historic progress in covering both children and young adults. In 2015, the uninsured rate for children fell below 5 percent for the first time on record. The uninsured rate for young adults (ages 19-25) fell to 15.8 percent, which is less than half the uninsured rate in 2010. These gains in large part reflect increases in the share of eligible children signing up for Medicaid and the Children’s Health Insurance Program (CHIP), as well the ACA’s provision giving young adults the option to stay on their parents’ health insurance until they turn age 26.
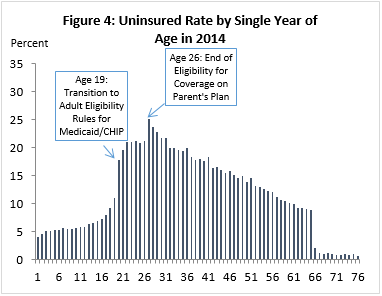
But recent data also show that, when young adults age out of Medicaid and CHIP at age 19 (the age at which young adults shift to being covered under the, generally narrower, adult eligibility rules) or turn age 26 and transition off their parents’ plans, too many of them are transitioning to being uninsured. Census data for 2014 show an almost 7 percentage point increase in uninsured rates at age 19, and an almost 4 percentage point increase at age 26 (see Figure 4). We are committed to flattening these cliffs and helping young adults stay covered.
Supporting Transitions at Age 26
When young adults turn 26 and “age off” their family health insurance, they need to take action to enroll in a new plan. For many young people, that means shopping for insurance through the Marketplace, where they are likely to qualify for tax credits to dramatically lower the costs of coverage. Thousands of young people successfully make this transition: in fact, 86,000 (60 percent) more 26- than 25 year-olds signed up for 2016 Marketplace coverage in HealthCare.gov states. But we also know there is more work to do.
Insurers can be critical partners in helping young adults navigate these transitions. Many young adults are covered under their parents’ employer-sponsored coverage, and that coverage is often facilitated by a company that also offers Marketplace health insurance. We encourage employers and health plans to work together to help their customers by providing young adults about to age out of their parents’ coverage with targeted information about Marketplace options.
Today, we are removing an obstacle that might have made it difficult for insurance companies to undertake targeted outreach to young adults about their options. Specifically, when a young adult ages out of their parents’ employer-based health insurance, the employer plan is required to send them a notice about the opportunity to enroll in COBRA continuation coverage or a Marketplace plan. But plans may have believed they were not allowed to do more, like help consumers through the enrollment process or give young adults information about the specific Marketplace products. New guidance from the Department of Labor makes clear that the sponsors of employer plans can – and are encouraged to – provide additional information that will help people understand their options and enroll in Marketplace coverage if it is right for them. This might include additional information about enrollment pathways, or even general information about specific products offered in the Marketplace. Employer plans can play an important role in helping young adults make a smooth transition between their family coverage and the Marketplace.
Supporting Transitions from Medicaid and CHIP
HHS is doing additional work this year to support children transitioning from Medicaid and CHIP to the Marketplace. In 2015, more than 42 percent of insured children were enrolled in public health coverage. However, when children become young adults and lose Medicaid or CHIP eligibility, the risk of becoming uninsured is unacceptably high. To ensure that young adults experience seamless transitions to other coverage options, the ACA requires effective coordination between insurance affordability programs. Young adults who age out of Medicaid or CHIP must be assessed for Medicaid eligibility under other eligibility criteria. In states that have expanded Medicaid, many young adults may be eligible for coverage under the new adult group. If ineligible for Medicaid, states are required to assess eligibility for a Qualified Health Plan through the Marketplace and transfer individuals as appropriate.
To maximize continuity of coverage for beneficiaries and reduce administrative burden, there are multiple steps that states can take. State-based Marketplaces with integrated eligibility systems can help individuals seamlessly transition from Medicaid to Marketplace coverage. Managed care organizations that provide both Medicaid and Marketplace plans can help states minimize disruption when individuals transition between coverage options. States can also enlist application assisters and Navigators to help young adults with the renewal process and potential transition to the Marketplace.
SECTION III: WORKING WITH PARTNERS TO REACH YOUNG ADULTS WHERE THEY ARE
HHS has created a network of diverse partners who are engaged in outreach to younger consumers. While we’ll keep building that network until the start of Open Enrollment in November and beyond, we are excited to announce today that our 2017 Open Enrollment partnerships will include:
Lyft
New this year, Lyft will develop user discount codes for people utilizing the ride-sharing service to attend Open Enrollment events where they can receive assistance signing up for coverage via the ACA. In addition, Lyft will again amplify enrollment deadlines and the importance of getting health insurance via the ACA to their drivers in 190 cities.
The American Hospital Association
The American Hospital Association
recognizes the importance of enrolling young adults in health insurance
coverage. They plan to develop a social media toolkit that hospitals may use to
reach young adults in their communities to educate them about health insurance,
how to enroll in their exchange, where to go for enrollment assistance, and
information about the subsidies. They also plan to promote hospital
incorporation of existing digital enrollment tools onto their websites, such as
the Get Covered Connector, to direct hospital website traffic to enrollment
assistance; and to develop messaging and materials for hospital to use about
the importance of maintaining and renewing coverage.
Partner Campaigns
Critical outside partners are coming together to lead targeted outreach through aligned strategies and coordinated messaging. Led by national partners like Enroll America, Young Invincibles and Out2Enoll, the 2016 campaigns will be:
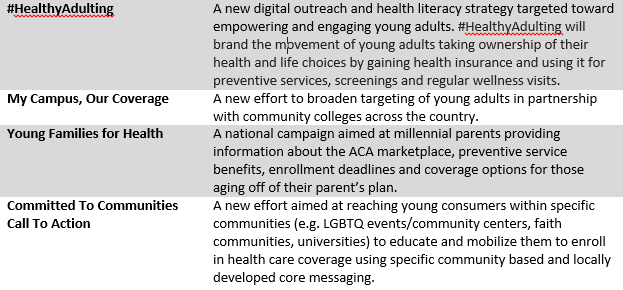
ACA Youth Coalition partners supporting these efforts include organizations such as Planned Parenthood, Urban League, America’s Health Insurance Plan (AHIP), Families USA, National 4-H Council, Boys and Girls Club of America, Campus Pride, Generation Progress, HOPE worldwide National Youth Advisory Council, YMCA, Islamic Relief, and United Way.
This outreach will also be supported by the National Coalition on Millennial Health – a newly mobilized coalition bringing together dozens of leading non-profits, advocates, hospitals and community health centers, insurers, and companies to create new outreach campaigns and develop the best research on expanding health care coverage and critical health services to young adults, ages 18 to 34. The first National Millennial Health Summit will be held at the White House on September 27, 2016 and this year’s National Youth Enrollment Day will be held on December 10, 2016.

No comments:
Post a Comment