... in
the U.S. are practicing in Primary Care, according to a recent report.
Source: "2014
Statistical Profile of Certified Physician Assistants by State: An Annual
Report of the National Commission on Certification of Physician
Assistants," National Commission on Certification of Physician Assistants,
Inc., January 2016, http://www.nccpa.net/Upload/PDFs/2014StatebyStateReport.pdf
At Medicare is Simple, we look to educate and enable you to choose among Medicare plans to help find the policy that may best fit your needs. Get free quotes using our advanced quoting technology. HealthCare Reform is also a hot topic of interest to people of all ages, and we look to keep you updated on the issues relevant to learning more. Medicare Is Simple 800-442-4915
Monday, February 29, 2016
"It is a totally random occurrence that when you change jobs it affects what insurance company you have...
... This is not
good for anyone. I should be able to vote with my feet and the insurance
company should get something out of investing in you because you know they
should over time earn that money back basically. Fundamentally, the
employer-based system is broken and over time it has to be individualized
through private exchanges or ACA exchanges."
— Mario Schlosser, CEO of Oscar Health, told AIS's Health Plan Week in an exclusive interview in his lower Manhattan headquarters.
— Mario Schlosser, CEO of Oscar Health, told AIS's Health Plan Week in an exclusive interview in his lower Manhattan headquarters.
During the two years leading up to the failed launch of HealthCare.gov in November 2013,
... HHS and CMS lacked leadership, which delayed key
decisions and caused a general lack of clarity in the development of the Web
portal, according to a report issued Feb. 23 by HHS's Office of Inspector
General (OIG). Additional missteps included devoting too much time to policy,
which left too limited time for developing the website. The report also
contends that CMS officials failed to heed multiple warnings that the
exchange's development was off track, according to the report. The report is
based on interviews with 86 HHS and CMS employees and employees of contractors
involved in the project. It also reviewed thousands of emails, contracts and
internal documents.
Friday, February 26, 2016
News for Federally-facilitated Marketplace Agents and Brokers - February 2016 Edition
An electronic source of information for
Federally-facilitated Marketplace (FFM) Agents and Brokers
In This Issue:
·
New
Resources for Agents and Brokers
o
Upcoming
Webinars
o
New
“Operational Updates and Announcements for Agents and Brokers Participating in
the FFMs” Webinar Slides Now Available
o
New
“Agent and Broker Roadmap to Resources”
o
“Operational
Tips for Agents/Brokers for Plan Year 2016 in the FFM”
o
New
Consumer Decision Support Tools Available at HealthCare.gov
o
Plan
Year 2016 Agent and Broker FFM Registration Completion List
·
Small
Business Health Operations Program (SHOP) Corner
o
The
SHOP Marketplace is Open All Year!
o
Second
Quarter Rates Available as of February 16
o
Have
SHOP Marketplace Renewals Coming Up?
o
New
Research Findings on Small Employers and the SHOP Marketplace
·
Special
Populations — New Parents and Their New Children Enrolling in the Marketplace
Outside of Open Enrollment
·
Spotlight
on Eligibility and Enrollment
o
Help
Consumers Understand the Application Question on Filing Taxes Jointly with a
Spouse
o
Help
Consumers Estimate their Expected 2016 Income
·
Did
You Know?
Reminding Consumers to Pay Their First Month’s Premium for Health Insurance
·
Follow
Us on Twitter
·
Contact
Us
New Resources for Agents and Brokers
Upcoming Webinars
CMS will be hosting a number of topic-focused
webinars in March on the following dates and times:
·
Tax Season Readiness 101: March 9 from 12:30 – 2:00
PM ET – This webinar will cover an overview of the forms, tips, and tools
agents and brokers should be familiar with as they help consumers prepare for
the 2015 tax season.
·
SEPs in the FFMs for Plan Year 2016: March 23 from 1:00 – 2:30
PM ET – This webinar will serve as a refresher on the availability of and
requirements around SEPs and changes in circumstances.
·
Assisting Consumers with Complex Situations: March 30 from 1:00 – 2:30
PM ET – This webinar will explain how to help consumers with multi-tax
households and family members enrolling in different qualified health plans
(QHPs).
To register for any of
the above webinars, log in to www.REGTAP.info and complete the
following steps:
1.
Select
"Training Events" from "My Dashboard."
2.
Select
the "View" icon next to event title for the webinar you are
interested in attending.
3.
Select
"Register Me."
If
you require assistance with webinar registration, contact the Registrar at
800-257-9520 from 9:00 AM – 5:00 PM ET, Monday through Friday or by email at: registrar@REGTAP.info. Registration
closes 24 hours prior to each event.
New “Operational
Updates and Announcements for Agents and Brokers Participating in the FFMs”
Webinar Slides Now Available
CMS has posted slides from weeks 12 and 13 of the
“Operational Updates and Announcements for Agents and Brokers Participating in
the FFMs” webinar series. Information about what each of these webinars covered
is available on the Agents
and Brokers Resources webpage. You can review the slides by selecting one
of the following sessions:
·
Week
12: January 19, 2016
·
Week
13: January 26, 2016
New “Agent and Broker
Roadmap to Resources”
CMS has released the Agent
and Broker Roadmap to Resources, which provides important information on:
·
The
Marketplace and other health coverage topics, and links to helpful resources on
those topics
·
Information
you need to know on how to help consumers apply for and enroll in Marketplace
plans and other health coverage
·
Coverage
options available to consumers
·
What
you need to know about the Marketplace Eligibility and Enrollment process to
help consumers get coverage
·
How
to access Marketplace information and resources in other languages
·
How
to get the latest information on Marketplace policies and operations
“Operational Tips for
Agents/Brokers for Plan Year 2016 in the FFM”
The updated Operational
Tips provides answers to agent and broker questions about consumer
enrollment for plan year 2016, including how agents and brokers can assist with
enrollments, the Marketplace 2.0 application, the Direct Enrollment Pathway,
reenrollment, capturing NPNs on an application, and registration.
New Consumer Decision
Support Tools Available at HealthCare.gov
The new consumer
decision support tools piloted earlier this enrollment season are now fully
deployed to all visitors to HealthCare.gov. These tools can help consumers more
easily search for the plans that best meet their budgets and health care needs.
·
The
Out of Pocket Cost calculator helps consumers better estimate the cost of their
health insurance based on their own personal situation.
·
The
Doctor, Facility, and Prescription Drug Look-up tools provide consumers with
easily searchable information about a plan’s networks of doctors and/or medical
facilities and the prescription drugs plans may cover.
Consumers will be asked to opt-in to use the tools to be sure they
understand limitations with the data. Agents and brokers can help consumers use
these tools when reviewing plans at 2016
Health Insurance Plans & Prices.
Plan Year 2016 Agent and
Broker FFM Registration Completion List
Check the Agents
and Brokers Resources webpage to view the most recent Agent and Broker FFM
Registration Completion List for Plan Year 2016, which includes the National
Producer Numbers (NPNs) of agents and brokers who have completed plan year 2016
registration requirements for the FFM as of the date listed in the filename. If
you completed registration after the date listed, check back and confirm your
NPN has been included when the new list is posted. Issuers can review the Agent
and Broker FFM Registration Completion List to confirm that agents and brokers
with whom they have agreements are authorized to assist consumers in selecting
plans through the FFM.
If you
completed all of the plan year 2016 agent and broker registration and training
requirements for the FFM, you should review the latest list to confirm your NPN
is included. You can search for your NPN by clicking the arrow in cell A1, or
by using the “Ctrl + F” (or “Command + F”) keystroke.
Small
Business Health Options Program (SHOP) Corner
The SHOP Marketplace
is Open All Year!
Open enrollment for individuals and families is over,
but small employers can still offer their employees’ health and dental
insurance through the SHOP Marketplace on a monthly basis throughout all of
2016. SHOP Marketplace applications submitted by the 15th of the month go into
effect as soon as the 1st of the following month.
Second Quarter Rates
Available on February 16
Plan for your SHOP Marketplace enrollments and renewals
for the upcoming year. In the SHOP Marketplace, the cost for health and dental
plans available may change on a quarterly basis for new enrollments.
As you get ready for your 2016 enrollments, please keep
the following key dates in mind:
·
February
16, 2016: SHOP Marketplace rates for the Second Quarter available
·
May
6, 2016: SHOP Marketplace rates for the Third Quarter available
·
August
16, 2016: SHOP Marketplace rates the Fourth Quarter available
Visit See
2016 Health Insurance Plans & Prices to view SHOP Marketplace health
and dental plans available at Healthcare.gov.
Have SHOP Marketplace
Renewals Coming Up?
You can begin assisting your clients with their renewals
as soon as the applicable quarterly rates become available, 45-60 days before
the renewal date. Your clients will also receive renewal notices from the SHOP
Marketplace around this time. For more information, visit HealthCare.gov.
New Research Findings
on Small Employers and the SHOP Marketplace
The Robert Wood Johnson Foundation commissioned research
to conduct focus groups and a national survey with employers with 50 or fewer
employees to understand their perspectives on offering health insurance, as
well as their awareness of and interest in the SHOP Marketplace. Notably, a majority
of small employers expressed an interest in enrolling in SHOP Marketplace
coverage when hearing about the benefits of the SHOP Marketplace.
You can download the study’s findings in a report or in
a recorded version of the webinar conducted on January 14, and view the
presentation slides on the new
research findings on small employers and the SHOP Marketplace.
Special
Populations — New Parents and Their New Children Enrolling in the Marketplace
Outside of Open Enrollment
Parents
who recently gave birth to, adopted, or are fostering children are eligible for
a SEP that will allow them to enroll in QHPs outside of the Open Enrollment
period. New parents may experience a change in coverage options or eligibility
for advance payments of the premium tax credit (APTC) and CSRs. Remind
consumers they should report such events to the Marketplace to find out what
changes the addition of children to their households might cause for their
coverage. For more information, check out the Helping New Parents and Their New Children Enroll in
the Marketplace Outside of Open Enrollment fact sheet.
Spotlight
on Eligibility and Enrollment
Help Consumers
Understand the Application Question on Filing Taxes Jointly with a Spouse
CMS has
added new language at HealthCare.gov to help consumers better understand
questions on the application related to household size, income, and how they
plan to file taxes. Consumers who indicate they are married, but do not plan to
file a joint federal income tax return with their spouse for 2015, will see the
following text to prompt them to consider whether they will file jointly:
If
you and your spouse are on the same tax return, select “GO BACK,” and change
your answer to “Yes” when we ask if you plan to file a joint federal income tax
return with your spouse.
If
you and your spouse aren’t on the same tax return, select “CONTINUE MY
APPLICATION.” If you file separately, you can’t get premium tax credits or
other savings, unless you meet certain specific exceptions. [Learn more about other tax filing circumstances.
Help Consumers
Estimate their Expected 2016 Income
When helping consumers fill out a Marketplace
application, it is important that you remind them that Marketplace savings are
based on their expected household income for 2016, not last year’s income.
Please take a moment to review the steps in the “How
to Estimate Your Expected 2016 Income” article on Healthcare.gov so you can
best assist consumers in estimating their expected 2016 income.
While you may provide
information to consumers about the APTC reconciliation process and the forms
that they will receive, it is important that you not provide any tax filing
advice or answer any tax filing questions. Please refer consumers seeking
answers to their questions or advice regarding their personal situations to a
tax professional for assistance or to the tax assistance options available at: IRS.gov/freefile or IRS.gov/VITA.
Did
You Know?
After
consumers have selected a new plan for 2016, they must complete one very
important task to finish enrolling — they must pay their first month’s premium
to their health insurance company, not to HealthCare.gov. As you continue to
assist consumers following Open Enrollment, please remind them to pay their
premiums to complete the enrollment process. It is important to note that each
issuer has different standards, so consumers need to pay careful attention to
their premium due date. For more information on helping consumers navigate the
payment process for their first month’s premiums, review the Healthcare.gov
Blog post, “Reminder: Don’t Forget to Pay Your First Month’s
Premium for Health Insurance.”
Follow
Us on Twitter
You can find important information
and updates by following the CMS and HealthCare.gov Twitter handles (@CMSGov and @HealthCareGov) or by searching for the hashtags #ABFFM or
#ABFFSHOP on Twitter.
Contact
Us
For questions pertaining to the FFM
agents and brokers program, including FFM registration requirements, or to
subscribe to this newsletter, please contact the FFM Producer and Assister Help
Desk via email at: FFMProducer-AssisterHelpDesk@cms.hhs.gov.
You may also contact the Agent and
Broker Call Center by calling 1-855-CMS-1515 (855-267-1515) and selecting
option “1.” Call Center Representatives are available Monday through Saturday
from 8:00 AM to 10:00 PM ET.
Agents/Brokers: Ready for Tax Season? Register for the Tax Season Readiness 101 Webinar
CMS will be hosting a “Tax Season Readiness 101” webinar for agents and
brokers on Wednesday, March 9, 2016 from 12:30 PM to 2:00 PM Eastern Time (ET).
The webinar will highlight information on how to assist consumers during the
2015 tax season and explain why consumers must reconcile advance payments of
the premium tax credit.
To
register for the webinar, please log in to www.REGTAP.info.
If you have questions on the webinar registration process, visit the new
“Upcoming Agent and Broker Webinars” section of the Agents
and Brokers Resources webpage for more information.
According to data from the January–September 2015 National Health Interview Survey,
...
after
adjusting for age and sex, the percentage of persons without health insurance
coverage by race/ethnicity was:
Source: "Early Release of Selected Estimates Based on Data From the January–September 2015 National Health Interview Survey," National Center for Health Statistics, Centers for Disease Control and Prevention, February 2016, http://www.cdc.gov/nchs/data/nhis/earlyrelease/earlyrelease201602.pdf
- 19.5%
for Hispanic persons
- 6.3%
for non-Hispanic white persons
- 10.0%
for non-Hispanic black persons
Source: "Early Release of Selected Estimates Based on Data From the January–September 2015 National Health Interview Survey," National Center for Health Statistics, Centers for Disease Control and Prevention, February 2016, http://www.cdc.gov/nchs/data/nhis/earlyrelease/earlyrelease201602.pdf
Thursday, February 25, 2016
Most Health Plans Provide Price Estimator Tools
America's Health Insurance Plans (AHIP) recently conducted a survey on health plan price transparency tools. Here are some key findings from the report:
·
Almost 3 in 4 health
plans surveyed provide price estimator tools to members.
·
39% of these plans
launched their price estimator tools more than 3 years ago.
·
4 in 5 of these plans
choose which services to provide estimates for based on common procedures.
·
Most (71%) health
plans provide estimates for physician services.
·
58% of plans included
cost estimates for prescription drugs.
·
2 in 3 responding
plans shared provider performance data with their enrollees.
Source: American Journal of Managed Care, February 16, 2016
"The roles of both [pharmacists and prescription drugs]...
... are often
overlooked in discussions of [accountable care organizations] despite the
widespread use of medications and the roles that pharmacists play in health
care delivery. Pharmacists are underutilized as trusted advisors to both patients
and physicians and other providers. The patient-facing role can be very
powerful in education and motivation...providing a potential solution to the
lack of patient engagement and commitment to self-care."
— Sharon Frazee, Ph.D., vice president of research and education at the Pharmacy Benefit Management Institute, discussing her institute's new report on pharmacy trends in ACOs at a recent PBMI webinar.
— Sharon Frazee, Ph.D., vice president of research and education at the Pharmacy Benefit Management Institute, discussing her institute's new report on pharmacy trends in ACOs at a recent PBMI webinar.
Wednesday, February 24, 2016
According to a recent study, 30% of outpatient visits ...
... included
conversations about health care cost, and 44% of these discussions included
cost-saving strategies.
Source: "What Strategies Do Physicians and Patients Discuss to Reduce Out-of-Pocket Costs? Analysis of Cost-Saving Strategies in 1755 Outpatient Clinic Visits," Medical Decision Making, abstract only, January 19, 2016, http://mdm.sagepub.com/content/early/2016/01/18/0272989X15626384.abstract
Source: "What Strategies Do Physicians and Patients Discuss to Reduce Out-of-Pocket Costs? Analysis of Cost-Saving Strategies in 1755 Outpatient Clinic Visits," Medical Decision Making, abstract only, January 19, 2016, http://mdm.sagepub.com/content/early/2016/01/18/0272989X15626384.abstract
The New Special Enrollment Confirmation Process
CMS BLOG
https://blog.cms.gov/2016/02/24/the-new-special-enrollment-confirmation-process/
February 24, 2016
By: Kevin Counihan, Health Insurance Marketplace CEO and Shantanu Agrawal, M.D., CMS Deputy Administrator and Director, Center for Program Integrity
The New Special Enrollment
Confirmation Process
At the end of January, we concluded our third Marketplace Open Enrollment Period with 12.7 million people enrolling in coverage nationwide – more than ever before. In addition, about 400,000 people are signed up on the New York and Minnesota Marketplaces for coverage through the Basic Health Program. Open Enrollment exceeded our expectations – four million new people enrolled in just the HealthCare.gov states alone, 60 percent of our new enrollees signed up before the January 1 coverage deadline, and 70 percent of returning consumers actively re-enrolled. Marketplace coverage is a product people want and need.
As the Marketplace continues to grow and mature, we continue to monitor the health of the Marketplace and are looking for ways to make improvements – whether that’s creating new decision support tools to help consumers choose the right plan, strengthening risk adjustment, or clarifying the rules of the road for special enrollment periods, as we did several weeks ago.
Today, we are announcing another step that will enhance program integrity and contribute to a stable rate environment and affordability for consumers: a new Special Enrollment Confirmation Process in the 38 states using the HealthCare.gov platform. Under the new process, all consumers applying through the most common special enrollment periods will need to submit documentation to verify their eligibly to use an SEP. This represents a major overhaul of the SEP process. You can read more about the Special Enrollment Confirmation Process here: https://www.cms.gov/Newsroom/MediaReleaseDatabase/Fact-sheets/2016-Fact-sheets-items/2016-02-24.html
Special enrollment periods are an important way to make sure that people who lose health insurance during the year or who experience qualifying life changes have the opportunity to enroll in coverage. We are committed to making sure that special enrollment periods are available to those who are eligible for them. But it’s equally important to avoid misuse or abuse of special enrollment periods.
This change in HealthCare.gov’s special enrollment period process does not restrict anyone's access to a special enrollment period who is rightfully able to enroll in coverage. But consumers will need to be sure to provide sufficient documentation to establish their eligibility. If an individual doesn’t respond to our notices, they could be found ineligible to enroll in Marketplace coverage and could lose their insurance.
As we begin work to implement the new process, CMS will solicit feedback from consumer advocates, insurers and other stakeholders over the next few weeks on verification requirements, processes and acceptable documentation. We welcome feedback and suggestions, which can be sent to SEP@cms.hhs.gov
As we head into the third year of Marketplace coverage, we are pleased with the results of Open Enrollment and confident that the Marketplace will continue to thrive for years ahead. Making sure that the rules around special enrollment periods are clear and enforced is just one step we are taking to help make sure that consumers and insurers will continue to benefit from an attractive, competitive and growing Marketplace.
Special enrollment periods (SEPs)
are an important way to make sure that people who lose health insurance during
the year or who experience major life changes like getting married or having a
child have the opportunity to enroll in coverage through the Health Insurance
Marketplaces outside of the annual Open Enrollment period. SEPs are a
longstanding feature of employer insurance, and without them many people would
lack options to maintain continuous coverage. But it’s equally important to
avoid SEPs being misused or abused.
At CMS, we are always monitoring
the health and operations of the Marketplace and looking for ways to improve.
We are focused on continually maintaining and refining a set of
Marketplace rules that create a healthy, stable and balanced risk pool.
Concerns have been recently raised about whether current Marketplace rules and
procedures are sufficient to ensure that only those who are eligible enroll
through SEPs. In response to that feedback, today we are announcing a new
Special Enrollment Confirmation Process that will address these concerns in the
38 states using the HealthCare.gov platform. These changes will enhance program
integrity and contribute to a stable rate environment and affordability for
consumers.
Once the new Special Enrollment
Confirmation Process is implemented, all consumers enrolling through the most
common HealthCare.gov SEPs will need to submit documentation to verify their
eligibility to use an SEP. The Special Enrollment Confirmation Process will be
accompanied by other improvements to the SEP application process, described
below. Today’s announcement represents a major overhaul of the SEP process.
Over the next few weeks, CMS will
invite comment from consumer advocates, insurance companies and other
stakeholders on the key features of the new Special Enrollment Confirmation
Process, such as communication with consumers, acceptable documentation, and
refining and targeting the verification process. These comments will help
inform implementation of the new process. This announcement builds on
action CMS has taken to eliminate unnecessary SEPs and clarify the rules for
other SEPs.
HOW SPECIAL ENROLLMENT
CONFIRMATION WORKS
Document Submission by
Consumers: Beginning in the next several months, all consumers who
enroll or change plans using an SEP for any of the following triggering events
will be directed to provide documentation:
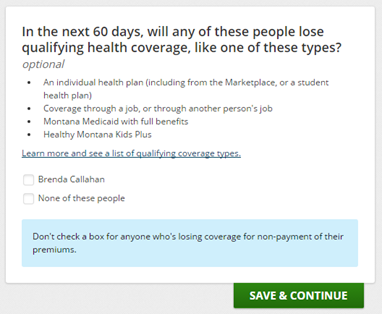
·
Loss
of minimum essential coverage,
·
Permanent
move,
·
Birth,
·
Adoption,
placement for adoption, placement for foster care or child support or other
court order, or
·
Marriage.
These SEPs represented three
quarters of HealthCare.gov consumers who enrolled or changed plans using an SEP
in the second half of 2015.
We will provide consumers with
lists of qualifying documents, like a birth or marriage
certificate. Consumers will be able to upload documents to their
HealthCare.gov account or mail them in.
Document Verification by
CMS: CMS will institute a verification process for consumers who
enroll or change plans using an SEP in 2016. The Special Enrollment
Confirmation Process is modeled after approaches used by the Internal Revenue
Service. We will review documents to ensure consumers qualify for an SEP and
will follow up with consumers if there is a question or problem. Consumers need
to be sure to provide sufficient documentation. If they don’t respond to our
notices, they could be found ineligible for their SEP and could lose their
insurance.
IMPLEMENTING THE SPECIAL
ENROLLMENT CONFIRMATION PROCESS
As we move forward with
implementing the Special Enrollment Confirmation Process, CMS intends to work
closely with our enrollment partners. In particular, we invite feedback on:
·
Communicating with consumers about providing required
documents:
As CMS implements the Special Enrollment Confirmation Process, we will work
closely with enrollment partners to ensure our notice language is clear about
what documents a consumer should submit and how those documents can be
submitted. We also invite feedback on best practices for communicating with
consumers regarding what documents can be used to establish eligibility for
different SEPs.
·
Refining the confirmation process: We invite feedback on how
our verification efforts respond to areas where there is the greatest risk of
SEP misuse.
·
Training assisters, agents and brokers: CMS will develop resource
guides for advocates, assisters, agents and brokers to help them understand the
Confirmation Process, acceptable documents, and situations in which consumers
do and don’t qualify for SEPs.
Feedback on the Special Enrollment
Confirmation Process should be sent to SEP@cms.hhs.gov.
WHAT ELSE CMS IS DOING TO
IMPROVE PROGRAM INTEGRITY FOR SPECIAL ENROLLMENT PERIODS
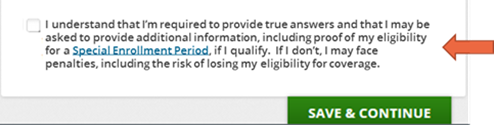
Requiring consumers to
acknowledge document request and reminding consumers of the need to be truthful:
In the next few weeks, HealthCare.gov will require all consumers who enroll or
change plans through an SEP to indicate they understand that documents will be
requested to verify their SEP eligibility. This process will begin in the
coming weeks and will ramp up over time and continue expanding once the Special
Enrollment Confirmation Process is fully in place. Consumers must also attest
at the end of their HealthCare.gov application that they are providing true
information and understand the penalties for misrepresentation. We’ll be
updating the application to include additional attestation language so that
consumers understand that they are required to be truthful and risk losing
their eligibility for Marketplace coverage.
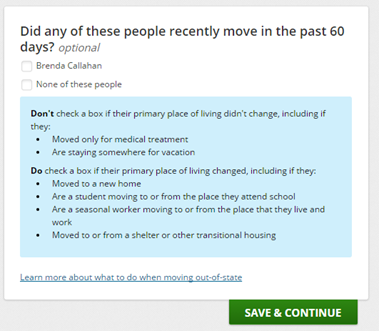
Clarifying application
questions for consumers: In the coming weeks, we’ll be updating
HealthCare.gov to make it clearer for consumers who are submitting or updating
an application to understand what does and doesn’t qualify as a loss of minimum
essential coverage, and a permanent move. Here are a couple of examples:
Call 1-800-318-2596 to
report Fraud or abuse: Anyone who suspects that there has been fraud
or abuse in the Marketplace should call 1-800-318-2596 to report their
concerns. Simply indicate that you are calling about fraud and abuse and
CMS investigators will receive the complaint.
86% ...
...
of large
employers will offer an account-based plan for 2016, according to an estimate
from Willis Towers Watson.
"The whole shift from fee-for-service to value-based health ...
...
is occurring
now, so that's why provider-sponsored plans are getting energized and why 25%
of all hospitals have said they're interested in starting a health plan. A lot
of them do start by focusing on the Medicaid or Medicare Advantage population
because these are institutions that are well-known in their community, they
have a really strong brand and these are their patients.... All those
populations that are more retail-focused or consumer-focused are natural
targets for a provider-sponsored plan because they don't have to prove who they
are."
— According to Bill Copeland, U.S. life sciences and health care leader for Deloitte LLP, and the author of a recent Deloitte study on provider-sponsored plans.
— According to Bill Copeland, U.S. life sciences and health care leader for Deloitte LLP, and the author of a recent Deloitte study on provider-sponsored plans.
Aetna Sees ACA Losses Improve, But Cigna Is Cautious on MA Woes
Reprinted from HEALTH PLAN WEEK, the most reliable source of
objective business, financial and regulatory news of the health insurance
industry.
By Patrick
Connole, Managing Editor
February 8,
2016Volume 26Issue 5
Aetna Inc. on Feb. 1 beat earnings
projections of Wall Street analysts for the fourth quarter of 2015, mainly on
stronger medical loss ratios (MLR) and improvement in individual and
small-group segments as well as impressive growth in its government business.
Most headlines centered on Aetna CEO Mark Bertolini’s comments during an
earnings call in which he questioned the sustainability of Affordable Care Act
(ACA) exchanges, going more negative on the marketplaces than he had in prior
exhortations for the industry to hold steady in the face of deep losses in the
first two years of exchange trade in 2014 and 2015.
“Our individual commercial business
ended the year with improved results over our most recent outlook. However,
despite our improved finish, this business remained unprofitable in 2015, and
we continue to have serious concerns about the sustainability of the public
exchanges,” he said. “Specifically, we remain concerned about the overall
stability of the risk pool, including enforcement of standards related to
special election period enrollment, where CMS has made some recent changes, but
more needs to be done.” Bertolini also cited the lack of predictability and
full transparency of the risk-adjustment program, “which is key to long-term
program health, especially as the other two premium stabilization programs
expire in 2017; and newly proposed CMS regulations on network adequacy and
standardization of benefits that would limit our ability to offer affordable,
innovative on-exchange products.”
Still, Aetna did realize better
operating results from the ACA-related individual segment in the fourth quarter
than previously projected, driven by improved medical costs and risk-adjustment
estimates. “Based on these updated estimates, Aetna’s individual commercial
business generated full-year 2015 pre-tax operating losses of approximately 3%
to 4%, a disappointing result, but one we are increasingly confident we can
improve upon in 2016,” Bertolini said. The goal is to get to break-even for the
$3.5 billion block of individual business as soon as possible, he stressed.
Overall, Aetna said net income rose to
$320.8 million, or 91 cents per share, in the fourth quarter of 2015, from $232
million, or 65 cents per share, in the same period of 2014. Operating earnings
were $1.37 per share, beating the consensus estimate of $1.21 per share. For
the same period of 2014, the insurer had operating earnings of $1.22 per share.
Vishnu Lekraj, senior equities analyst
for Morningstar, Inc., tells HPW there were not many surprises in
Aetna’s results, but did note ACA-market developments. “They did a little
better on the exchange market than what people were expecting. But nothing is
going to develop until we see how the exchanges shake out as far total signups
and how well the M&A [Humana Inc. takeover] is progressing for them,” he
says.
Some more clarity did come on ACA
enrollment from the Obama administration on Feb. 4, however, when it said about
12.7 million people had signed up for coverage this year. That number is in the
range of the administration’s stated goal of between 11 million and 14.1
million enrollees. Still, the 12.7 million is only 1 million more than signed
up in 2015. And by the end of this year, the White House target is to have 10
million enrolled, accounting for dropouts throughout the year.
With all the discussion about health
insurer losses on exchanges (see brief, p. 7), and threats by the likes of
UnitedHealth Group to exit the marketplaces next year if things don’t improve (HPW
11/23/15, p. 1), there are voices defending exchanges. For instance, Peter
Lee, executive director of the Covered California exchange, put the onus on
insurers to shape up their strategies. “Plans on exchanges, whether in
California or outside, should be pricing to make a reasonable margin,” he tells
HPW sister publication Inside Health Insurance Exchanges. “Our
plans have reasonable margins in California. And most plans have had reasonable
margins nationally. If a plan doesn’t have the acumen or strategy to make it
work on an exchange, they shouldn’t be playing.”
Beyond ACA exchanges, analysts looked
to Aetna’s underwriting acumen as a big reason for its positive fourth quarter.
“Earnings per share was driven by better-than-expected underwriting margin
across both commercial and government programs,” said Matthew Borsch,
securities analyst for Goldman Sachs - Global Investment Research, in a Feb. 1
note. He said total MLR of 81.9% for the fourth quarter of 2015 was better than
the 82.7% consensus. Medicare and Medicaid MLR did even better, coming in at
82.6% for the fourth quarter of 2015 versus the Wall Street estimate for 84.5%.
Cigna Sees Uneven MLRs, but Beats
Street
Also reporting fourth-quarter 2015
earnings was Cigna Corp., which on Feb. 4 told investors it made more money
than Wall Street forecast for the final stanza of last year. Still, the insurer
said net income declined to $426 million, or $1.64 per share, in the fourth
quarter of 2015, from $467 million, or $1.77 per share, in the same period one
year earlier. But on an adjusted basis, net income was $1.87 per share,
eclipsing the average analyst estimate of $1.80 per share.
For this year, results are expected to
be hurt by an ongoing CMS suspension of Cigna’s Medicare Advantage marketing
and enrollment due to what the agency called “widespread and systemic failures”
in allowing members to access medical care (HPW 2/1/16, p. 7). Still,
Cigna dodged a bullet with CMS’s timing, since the Annual Election Period had
already completed by Jan. 21 when CMS levied the sanctions. Cigna put its 2016
profit forecast at $8.85 to $9.25 per share, well off the Wall Street estimate
for $9.30 per share.
Equities analysts said on the surface,
the performance by Cigna was “solid,” but a little digging put the results in a
lesser light. “Beneath the surface, the Medicare MLR was challenged a bit and
while reserves on a year-to-date basis continue to be solid, there appeared to
be a modest reduction in conservatism sequentially whereas peers have been
building reserve positions in 4Q15,” said Brian Wright, securities analyst for
Sterne Agee CRT in a Feb. 4 research note.
Cigna said its consolidated MLR was
81.4% for the fourth quarter, topping the Wall Street consensus estimates of
81.6% by 20 basis points; it also represented a 20 basis points improvement
from the same period of 2014. “The Commercial MLR at 80.4% was 90 basis points
better than the 81.3% consensus estimate. The results were better despite
continued high medical cost in the U.S. Individual business. The Government MLR
of 83.1% was 140 basis points worse than consensus estimates of 81.7%, due to
pressure in their Medicare Part D business,” he said.
Wright added that the pending Anthem,
Inc. acquisition of Cigna reduces the importance of slight “nuances” in Cigna’s
quarterly results. Separately, Wright said the expectation remains for the Anthem-Cigna
deal to close in the second half of this year.
https://aishealth.com/archive/nhpw020816-03?utm_source=Real%20Magnet&utm_medium=Email&utm_campaign=90677619
Subscribe to:
Posts (Atom)